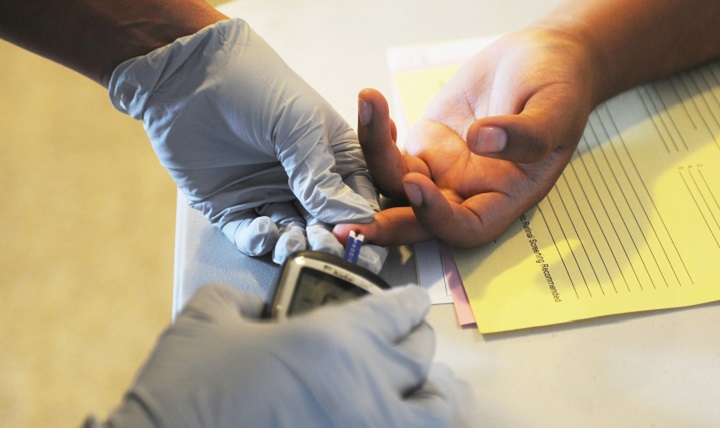
How many times have you read an article that said “avoid these foods if you have diabetes” or “if you are prediabetic?” The truth is, almost all of this information is referencing type 2 diabetes, as it’s more common than type 1.
In fact, of the 30.3 million Americans who have diabetes, an estimated 90 to 95 percent of these individuals have type 2. However, each type requires different treatment and management.
To explain the difference between type 1 and type 2 diabetes, we consulted endocrinologist Dr. Kathleen Wyne of The Ohio State University Wexner Medical Center, so you never confuse the two ever again.
What is the difference between type 1 and type 2 diabetes?
Someone with type 1 diabetes cannot make a hormone called insulin, whereas someone with type 2 diabetes can, but they don’t make enough to keep their blood sugar levels in check.
”People with type 1 diabetes need to be on insulin at diagnosis or they can die from DKA,” says Wyne.
DKA stands for diabetic ketoacidosis, a fatal complication that occurs when insulin is absent in the body. A person who has type 1 diabetes is inherently deficient in insulin because the beta cells in the pancreas that are responsible for producing insulin have been destroyed.
As a result, insulin injections are necessary to ensure that cells aren’t deprived of glucose (sugar), their energy source.
Insulin helps to transfer glucose to these cells, but when insulin isn’t there, the body begins to break down fat and uses that for fuel. If left untreated, acids called ketones can begin to build up in the bloodstream which then can lead to DKA. This is why it’s vital for those with type 1 diabetes to receive insulin either from a pump or a shot.
According to the USDA, there are five types of insulin.
- Rapid-acting. This insulin begins working within 15 minutes of using it. The best time to use it is right before or right after you eat to prevent a spike in blood sugar.
- Short-acting. This insulin will work between 30 minutes and one hour of using it. It’s best used 30 to 45 minutes before you eat.
- Intermediate-acting. This insulin begins working between two and four hours after using it. It’s used as a means to help control blood glucose levels between meals.
- Long-acting. This insulin also begins to work around two to four hours after taking it, but it can last in the body for up to 24 hours.
- Pre-mixed. Aptly named, this insulin is a mix of two different kinds of insulin: one that helps control blood glucose levels during meals and one that helps in between them.
“The goal of insulin therapy is to mimic what the actual pancreas does,” says Wyne. “This means that people with type 1 diabetes need a long-acting insulin to be working in the background or an insulin pump, providing a continuous low-level infusion, and a fast-acting insulin with all meals and all snacks.”
Someone with type 2 diabetes, on the other hand, can secrete insulin. However, one of two complications are thought to occur. Essentially, either the pancreas cannot secrete enough of the hormone to allow glucose into all of the cells that need it, or the pancreas is working overtime to produce more of the hormone because the cells have become resistant to it and as a result don’t allow glucose in.
Wyne says that the most significant risk factor of type 2 diabetes is having a family history of it. On the contrary, only one-third of all newly diagnosed type 1 diabetes patients know a family member with the condition.
“However, the disease physiology is very complicated, thus, there are many places where a defective gene could cause or contribute to type 2 diabetes,” she adds.
People who have the following metabolic disorders are also at greater risk of developing type 2 diabetes:
- Hypertension
- Mixed dyslipidemia
- Fatty liver disease
- Cardiovascular disease
- Obesity
Type 2 diabetes can be managed through diet and exercise, but in some cases, additional insulin is needed.
What is prediabetes?
Prediabetes is the precursor to type 2 diabetes. According to the most recent report from the CDC, about 84.1 million Americans have the condition. Prediabetes can be reversed through lifestyle changes such as cutting back on calories, losing excess weight, and committing to regular exercise.
“It is meant to be a warning sign that action needs to be taken immediately and not meant to be considered a chronic disease entity that one would treat with a pill,” says Wyne.